Dr. Mauk’s Boomer Blog
Each week, Dr. Kristen Mauk shares thoughts relevant to Baby Boomers that are aimed to educate and amuse.
Dr. Kristen L. Mauk, PhD, DNP, RN, CRRN, GCNS-BC, GNP-BC, FAAN

Guest Blog: 5 Tips for Finding a Life Insurance Policy that Works For You
In a world full of uncertainties, it is important to ensure your protection and that of your loved ones are guaranteed. A life insurance policy is a legal and mutual contract between you and a life insurance provider. In a life insurance policy, the insurer is called upon to make certain payments of money and list down beneficiaries who will benefit from the program if the insurer dies off in case of an unfortunate happening.
One of the biggest financial decisions you will ever make is signing up for a favorable life insurance policy that will wholesomely come through for you in any tight situation. The following are tips for finding a favorable life insurance policy:
1. Assess the Current Financial Situation You’re in
Before settling on a life insurance policy, you have to have a definite picture of your financial health. Assess the total amount you have that will cater for your family members, which includes:
- Monthly income
- The emergency funds available
- The life insurance coverage via work
- The retirement savings.
You may add up all the assets and find out that you are not eligible for a life insurance program. To ensure you make the right decisions, you should work with a financial planner to help you decide what needs to be safeguarded by the life insurance policy.
2. Understand What Affects Your Life Insurance Rate
When deciding on the rate, you need to pay for coverage; the key factors looked at by life insurance companies are your health and age. The younger you apply for your life insurance, the cheaper the life insurance rates are. This is because people are mostly healthy when they are young and run into fewer risks that push them towards applying for insurance policies.
The type of policy granted to you and the death benefits hugely depends on the rates paid by you. Most life insurance policies have an option for you to convert a term life insurance policy to a permanent insurance policy as desired with an increase in your income.
3. Choose an Insurance Policy Type
When planning to buy a life insurance policy, you have the option to choose between a term policy and a whole life insurance policy. A term policy is an advantageous way to help you cover bills such as mortgages or your kid’s education because they are only for a while.
However, a permanent life insurance policy is long-term with lifelong coverage. Compared to a termed insurance, permanent life insurance is expensive because of its high cash value. The cash is useful in supplementing retirement income or during emergencies.
4. Assess Your Life Insurance Goals
Every person has different goals and intentions with their insurance policies. With the aid of a suitable insurance policy, you have to formulate your goals well and ensure the amount you are directing to the insurance company can comfortably fund your goals without inadequacy. Whether it is a team or lifelong insurance, Omaha Insurance Medicare Agent ensures your assets are safe and all the goals are met at the end of the day.
A unit-linked insurance plan helps you take care of matters such as your child’s education and purchase a retirement plan that guarantees your daily expenses after retirement. Also, it is crucial to set realistic goals depending on the income you generate.
5. Name Your Life Insurance Beneficiary
A life insurance beneficiary is a person who benefits from the proceeds of your insurance policy. When choosing a beneficiary, it is important to choose wisely as this is the individual who will reap the fruits of your labor when you are not around. You can contact an independent agent to walk you through choosing your beneficiary.
When choosing a beneficiary, avoid opting for minors or infants that may fail to receive the funds. Also, avoid naming an estate as a beneficiary because it may go through tax implications, and you end up not benefitting from the insurance you worked hard to save for.
When going through the life insurance applications, ensure you have someone with your best interest in mind so that you can make sober decisions. While tapping into life insurance, you have to be intentional with the plans you have and prioritize paying the stipulated amount so that when the time comes for you to withdraw the money, you have something that can guide you to the next step in life.
Mastering your medical paperwork: Tips from a professional organizer
By Radha at Inspire
Inspire is a leading social network for health that connects patients and caregivers in a safe permission-based manner
Mastering your medical paperwork: Tips from a professional organizer
Who knew getting sick could require the combined skills of a librarian and an archivist? For most of us, managing the paperwork that comes with medical care can be an overwhelming task.
“In so many ways, you’re powerless,” said J.J. Jackson, an organization professional in the Washington D.C. area and owner of PaperworkMaven.com. “Especially people who have a lot of doctor’s appointments, they’re really sick and just don’t have the energy to do all this stuff… It’s so frustrating and it takes emotional time.”
Getting on top of medical paperwork – mainly, knowing where things are, what is complete, and what is not – can help people reclaim some power.
“It definitely empowers me,” Jackson said, because tracking her information gives her a complete picture of her medical and financial situation and she can speak with confidence about tests, needs, and money paid and owed.
Organized medical paperwork can also reduce stress and even save money. If you’re struggling to keep medical paperwork organized, here are 5 easy tips from a professional organizer.1. Put everything in one place
1. Put everything in one place
At minimum, having everything together is critical, Jackson said. This could be the point where some people stop; it might be a starting point for others to organize further. But as long as everything is in one spot – a box, a folder, a digital file – you can get to it later.
2. Set aside time for paperwork (it’s probably less than you think)
Time is the number one thing that Jackson said gets in her way.
For someone who has regular medical appointments and a paperwork backlog of several months, Jackson estimated about three hours of concentrated work to organize paperwork into a system. However, once the system is in place, it may require less than 30 minutes per week to log and file new information. In her experience, Jackson said calling insurance companies takes up the most time.
3. A Table of Contents is your best friend
Ideally, a system for paperwork would have an easy-to-skim main document to which related materials like receipts, Explanation of Benefits statements, medical reports, and images can be traced. This also makes it easy for others to figure out your medical picture, if necessary. It can be physical or digital.
Through her personal and professional experience, Jackson created a simple spreadsheet to track claims, a few claim details, and payments. Each line item corresponds to one day. Jackson labels related documents with the same line-item, so she knows what claim they correspond to. She won’t check off a line item until each task and payment associated with it is resolved.
“It’s about making sure you have enough detail to track things needing attention and things that are done,” she said,
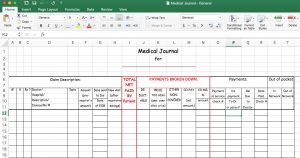
Create a chart to organize and track your medical paperwork.
4. Delegate
Many people don’t realize they can and should delegate paperwork-related tasks. But, Jackson said, consider that having your medical paperwork in order is important enough to devote resources to it.
“I think people think they ought to be able to do it themselves,” she said. “It’s ok if you don’t want to do it. If someone is sick, I think it would be such a gift to them. If they just don’t have time or energy or the emotional capability doing that, as a family member or friend, that is an excellent gift to give.”
Expert resources from organizations like the National Association of Productivity and Organizing Professionals and the American Association of Daily Money Managers could be of use said Jackson, who enlists help for medical tasks herself. And depending how comfortable you are letting others see sensitive personal health information, hiring someone to sort, log, file, and do general paperwork-related tasks could also help.
5. Physical vs digital systems
Digital organization and cloud storage will be the way of the future, Jackson said. The challenge right now is that medical information is spread over multiple locations and multiple types (paper receipts and reports, emails, digital image files, audio recordings, and personal notes, to name a few) and there aren’t good ways to integrate these in one system.
Jackson has separate locations for physical and digital materials but sticks to the same labeling system that corresponds to her main chart. If you’re really committed to a paperless system, a good scanner is essential, Jackson said. A robust organization system should accommodate how you like to store and track your materials and adapt to changes in health needs over time.
Except for those who enjoy detailed organization work, Jackson admits getting medical paperwork organized is not fun. Rather, it’s a means to an end.
“The feeling I get when I’m done is really satisfying,” she said. “I feel accomplished and I feel empowered and like I have peace of mind.”
10 Things to Consider Before Moving to a Care Home
A care home makes up for one of the best places to access assisted living services. There are many such services in the country, making it difficult to choose the right one. You have to consider many unique factors to ensure you choose the ideal service provider. Fortunately, this guide looks at ten things to consider before moving to a care home:
1. The Pricing Packages
A care home offers services at a cost, and you have to be aware of their pricing plans. Usually, each pricing plan comes with different offers and levels of assisted living benefits. Reviewing these plans will help you make an informed decision for your care home needs. You can request information such as the average cost of assisted living by calling the care home or vising their website. Ensure you ask all relevant questions about each pricing plan before investing.
2. Online Presence
A good assisted living service is available online because nowadays, the average person uses the internet to search for solutions. The service should be available on social media, a website, or any other internet-based platform. A simple search engine query should help expose all the relevant care homes in your location. The ones that come up high in the search results are usually the most reputable.
3. Location
Logistics is a crucial factor when choosing the ideal care home. People have different location needs, and you have to consider this in choosing the ideal home. Some prefer homes that are in urban areas, while others prefer those that are in reserved locations. The location also helps determine whether you have chosen a reputable service because unprofessional people tend to work in remote areas.
4. Regulatory Approval
A care home should run as a state-recognized and approved business entity. Usually, the evidence of this approval is available on the business’s website or product portfolio. Or, it can also be available through local state databases or records. The approval helps to show that you have chosen a professional service.
5. Medical Services Offered
People in care homes sometimes need various types of medical services. A good care home can address these needs and suits the need of different patients. Medical services can include prescription management, mental health initiatives, and more. You also have to determine whether the home has the licensing to offer such services.
6. Enhanced Assisted Living
Enhanced assisted living refers to the various technologies a care home offers to patients with special needs. A good example would be assistive devices that help deaf patients or those with memory loss. The devices help these individuals to navigate everyday obligations conveniently. While such resources are likely to increase the cost of medical care, they are crucial for assisted living purposes.
7. Team of Staff
The team of staff available at the care home is also crucial for the assistive living services they can provide. Ensure you have a broad perspective of each team member before settling on a specific service provider. Doing this will help increase the likelihood of receiving high-quality medical health attention or help. It also helps ensure that the facility well addresses each patient’s needs.
8. Offers and Incentives
The quality of incentives the care home provides is also crucial for the medical services to its patients. The offers and incentives should be transparent and suitable for patients with long-term needs. The reason is that most care home patients are patients who will live in the facility for long durations. The offers can include discounts and privileges such as vacations for loyal clients.
9. Affiliations
You should also consider a care home with excellent affiliations with entities such as medical facilities. The reason is that it helps guarantee the likelihood that you will receive high-quality care home services. The affiliations can include those that exist with traditional medical services.
10. Social Support Programs
The ideal care home also has excellent social support programs for its patients. The programs should include recreational, physical, and other forms of outdoor activity. It should also include custom programs for people that have specific care needs.
Conclusion
As you have noticed, there is more to receiving medical care than the average person can expect. You must consider various factors and details to ensure you get the best service provider.
Constipation Treatment
Background
Constipation is the most common bowel problem in older adults. The definition varies by patients and health care providers, but generally it means less frequent bowel movements than usual, and those which are hard, dry, and difficult to pass. Constipation is a preventable and treatable problem. Changes that occur with normal aging, such as peristalsis in the gut slowing down or decreased physical activity, predispose older persons to constipation.
Risk Factors/Warning Signs
Constipation is often due to a combination of causes. Some of the risk factors include decreased activity, medications (such as certain pain pills, iron supplements, and calcium supplements), depression, neurological conditions (dementia, Parkinson’s disease, stroke, diabetes mellitus, and spinal cord injury), dehydration, low dietary fiber, metabolic disturbances (such as hypothyroidism), undergoing dialysis, obstruction, and decreased access to the toilet (Halter et al., 2009). The range of “normal” for bowel movements is three times per day to three times per week. A decrease in number of stools that is “normal” for the person and the occurrence of hard, dry stools that are difficult to expel are typical signs of constipation.
Diagnosis
If constipation is severe enough for the person to seek medical care, the patient may complain of abdominal pain and even have symptoms similar to other problems such as an appendicitis or diverticulitis. These more serious ailments can be ruled out through x-rays, CT scan or MRI. The diagnosis is based on clinical presentation, history, and physical examination. It is important to determine the onset and duration of the constipation, along with functional and nutritional status.
Treatments
Before starting a bowel program to prevent constipation, the existing problem should be dealt with. A physician may prescribe laxatives, suppositories, and/or enemas to get the stool moving and eliminated. Many such products can be obtained over the counter as home remedies, but severe and recurrent problems should be referred to the primary care provider for further examination of the cause. After starting with a clean bowel, interventions should focus on lifestyle and dietary modifications. All natural means should be tried first before adding medication to the regimen. This includes regular exercise, establishment of a regular routine for toileting (assure privacy), and encouragement of a high-fiber diet with adequate fluid intake (unless contraindicated)(Joanna Briggs Institute, 2008). Medications may be considered for those who do not respond to lifestyle changes. Residents of nursing homes appear to respond to stimulant laxatives (e.g., senna, bisacodyl) or Miralax. Enemas should not be used on a regular basis because they promote lazy bowel function. Most older persons can avoid constipation if they remain active, have proper nutrition high in fiber, and drink plenty of fluids.
Adapted from Mauk, K. L., Hanson, P., & Hain, D. (2014). Review of the management of common illnesses, diseases, or health conditions. In K. L. Mauk’s (Ed.) Gerontological Nursing: Competencies for Care. Sudbury, MA: Jones and Bartlett Publishers. Used with permission.
http://www.mayoclinic.com/
Guest Blog: Tools to Make Your Shower Safer
Have you heard? A new government study has revealed that falls among adults over 65 rose over 30% in the past 10 years! While a fall every now and then may feel like no big deal, it is important for seniors to recognize that even seemingly harmless falls can lead to dangerous complications like hip fractures and head trauma.
If you or the person you care for hasn’t fall-proofed one of the most dangerous spots in the home, the shower, yet, don’t miss this essential list of helpful safety tools:
Toiletry Dispenser
Are you still struggling with slippery bars of soap and hard-to-grip shampoo and conditioner bottles in the shower? Get an easy-to-install toiletry dispenser instead which can stay fixed to the wall under your shower head and dole out toiletries in your hand as needed with the push of a button.
Grab Bars
Experts recommend installing grab bars both inside and outside the shower on walls that are easy to reach and can fully support your weight when you brace against them. Similar products like bathtub bars which sit fixed on the side of a bathtub and provide a raised support to hold and steady yourself are great too for notoriously hard-to-navigate tub showers.
Non-slip Shower Mat
Not all shower mats are created equal, and for seniors taking fall prevention measures in the shower, finding one that stays in place and offers a textured non-slip surface to stand on is critical. Additional features like being antimicrobial and machine-washable also prevent the buildup of contaminants and mildew which are common to humid areas like the shower.
Shower Chair
Even if you have no mobility issues at all, a shower chair may be a good investment if your space allows for it. Shower chairs make it easy to sit and rest in the shower if you suddenly feel weak or unbalanced. And specialty transfer chairs help caregivers easily get a loved one in and out of the shower without over-exerting themselves or putting their loved one’s safety at risk.
Handheld Shower Head
Quit trying to twist, turn, and contort your body when bathing yourself. A removable, handheld shower head is a must for easy, thorough washing that won’t leave you with a muscle strain in your back. Experts recommend getting one with at least 5 feet of maneuverable cord to allow for enough slack to raise and move it around your body with ease.
Outside of the shower, additional upgrades that can improve your safety and bathroom experience include automatic lights that provide consistent, bright lighting without having to flip a switch, non-slip bathroom mats, and raised toilet seats with handles.
Guest Blog: Common Signs of Hearing Loss
Hearing loss can have a profound effect on a person and their quality of life. Hearing loss can lead to a withdrawal from social situations, signs of depression and other effects on the health of an individual. Therefore, it is imperative that any loss in hearing be treated as soon as possible. In order for hearing loss to be treated, an individual must recognize that a loss of hearing has occurred. Some hearing loss can have a gradual onset, so the person with the hearing loss may not be fully aware that treatment is needed.
According to the National Academy on an Aging Society, millions of Americans suffer from hearing loss. Those suffering from hearing loss range in symptoms from very mild to severe or near total hearing loss. Of these, 43 percent are those individuals aged 65 and older. However, hearing loss can affect all ages with some 5 percent of children having some form of hearing loss. The causes of specific hearing loss are varied, with some created due to occupational stress, or life choices, or those brought about because of aging.
Audiologists and hearing aid specialists at Hearinglife.com lists the types of hearing loss as:
- Conductive Hearing Loss
- Sensorineural Hearing Loss
- Mixed Hearing Loss
Conductive hearing loss is a result of some form of obstruction in the ear. This type can be temporary and usually corrected via medical procedure and occasionally the application of a mechanical aid.
Sensorineural hearing loss is damage or some other issue affecting the auditory nerve or inner ear. This category encompasses hearing loss due to aging or disease. Correction usually involves the application of assisted hearing devices as this loss is usually permanent.
Mixed hearing loss is attributed to directed sound at excessive volume, such as that found in headphones and in occupational settings. Corrective measures also require the use of a mechanical or assisted hearing device. Based on statistics performed by the Centers for Disease Control and Prevention, mixed hearing loss is a widespread concern affecting over 22 million Americans each year. As suggested by the professionals for Kaiser Permanente Health System, they symptoms of hearing loss appear as:
- Muffled Hearing
- Requiring Higher Than Normal Volumes
- Frequently Misunderstanding Spoken Words
- Ringing or Pain in the Ear or Fluid Leakage
- Off Balance or Feeling of Spinning
Any of these, and potentially other symptoms, can occur with hearing loss. Even before hearing loss is suspected, it is generally accepted that hearing should be tested regularly in order to quickly diagnose and treat any hearing loss before it becomes significant to the detriment of the individual and their quality of life.





