Recent news and updates
Dental Implants for Seniors – A to Z explained
When you get older, it’s common to wonder if dental implants are the best option for you. You might consider the success percentage of your implant procedure given your age. It’s possible to wonder if dental implants are equally effective for elderly individuals as they are for younger ones.
Fortunately, dental implants are just as durable and effective as ever as people age. Dental implants frequently improve the physical and psychological well-being of elderly persons, as well as their sense of self. There is no maximum age for dental implants.
Implants can also be used for Dentures and Bridges.
Implant Retained Dentures Ill-fitting and loose dentures can be a major issue. You don’t have to make sacrifices by modifying your diet, eating soft foods, or avoiding certain social events – an Implant Retained Denture is a cost-effective method for replacing a full set of teeth. Implant Retained Dentures are more reliable and functional than standard dentures, allowing you to consume the things you enjoy without worrying about your teeth falling out.
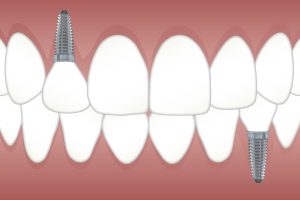
Implant Supported Bridge An implant-supported bridge is identical to a traditional dental bridge, except that it is supported by implants rather than natural teeth. When an implant-supported bridge is used, an implant is typically inserted in the jawbone for each lost tooth. The crowns are then joined together to make one piece.
How Do Dental Implants Work?
Dental implants resemble false tooth roots that are screw-shaped. Dental implants will be inserted into your jawbone by a skilled dentist and will fuse with your natural bone over time. This serves as a foundation for crowns, which are prosthetic teeth.
To hold your crown, a connection, sometimes referred to as an abutment, is put on top of the dental implant. The crown is designed specifically for you to fit in your mouth and match your teeth.
The strongest, safest, and most reliable dental operations are dental implants.
What to Expect When Getting Dental Implants
Several steps are often involved in dental implant procedures:
Consultation – A qualified professional like an implant dentist in Docklands will inspect your mouth, take 3-D X-rays, and discuss implant choices with you before determining the best course of action for your dental implant procedure.
Placing Dental Implants – Your dentist will place the dental implant in your jaw at your subsequent appointment, exactly where your missing teeth should be. Most patients have less pain and discomfort than anticipated and typically go back to work the next day.
But remember that every person has a different experience. In order to make you more comfortable during surgery, IV sedation or local anaesthetic may be utilised.
Similar to other dental surgeries, post-implant surgery discomfort exists. It could cause pain, bruising, swelling, or mild bleeding. Most people typically use over-the-counter drugs to treat any pain.
Osseointegration – Osseointegration is the process that occurs when your dental implant and jawbone begin to grow together. A solid and durable foundation is created throughout this process for your new teeth.
Your dentist might recommend a soft food diet for a few weeks to ensure that your implants recover properly. You’ll return to your regular life in a few months.
Placing an Abutment – Your dentist will attach a small connector to the dental implant (an abutment) after the implant has established a relationship with your jawbone. In some circumstances, the connector can be implanted at the same time as the implant.
Add Fresh Teeth – Your dentist will custom-make your new artificial tooth once your gums have recovered from the initial procedure by taking impressions of your mouth using your natural teeth.
A single crown, a bridge supported by implants, or dentures with several replacement teeth can all be created by the dentist. Though they won’t decay, your artificial tooth or teeth will still require the same regular maintenance, checkups, and cleanings as with genuine teeth.
Check-ups – The number of artificial teeth placed and the type of implant you receive will determine how frequently you will need to have your dental implants evaluated. Typically, the entire procedure takes three to nine months.
Regular follow-up visits with your dentist are expected to ensure that everything is recovering properly.
Taking Care of Dental Implants Following the Procedure
Following dental implant surgery, you should anticipate:
- Your gums and face swelling
- Minor bleeding
- your skin and gums becoming bruised
- the implant location hurts
Usually, the dental surgeon will employ self-dissolving stitches. Your doctor removes your stitches if they do not dissolve on their own. Your doctor might advise you to take antibiotics or painkillers.
Guidelines for Maintaining Your Dental Implants
Seniors who receive dental implants typically have success. The bone may not always fuse to the dental implant. The dental implant is taken out in these situations, and you can try again in around three months.
Your implants will last longer if you:
- maintaining a regular oral hygiene routine that includes brushing and flossing
- Regularly seeing your dentist and receiving specialized cleanings
- Avoiding bad habits like smoking, chewing ice or hard candy, and
Remember that there is a slight chance of bleeding issues, infections, and allergic responses with all oral operations. For example, if an implant is positioned too close to a nerve, it may result in tingling or numbness in the face, lips, tongue, or gums. The dental implant site may experience discomfort, edoema, fever, and chills if your body rejects it.
After receiving your implant, you should visit the dentist again right away if you notice any symptoms or think there might be a problem.
Luke is the owner and clinical director at Royal Wharf Dental. His vision for the clinic was to create an environment and an experience unlike any other, with an attention to detail and delivery of service surpassing all expectations.