Kidney Stone versus Labor – And the Winner is?
I had always heard that kidney stones were the closest thing to labor pain and childbirth that a man could experience, but being a woman who had been through labor four times, I didn’t quite believe it or understand the comparison. That is, until the other day…
I was sitting at the computer writing and felt a pain like a muscle cramp in my right side. But, since I couldn’t recall having done anything strenuous the day before, I just figured I had been sitting too long in one spot. Moving around helped for a brief time until the pain returned, more intense and radiating from the right flank around my side and down to my groin. Hmmm….being a nurse I wondered what this could be so I tried the usual techniques as the pain intensified: Tylenol, the massage chair, walking, lying down, sitting up, and having the kids rub my back. Yikes, the pain that can only be described as an unrelenting, constant hurt of the greatest magnitude, a 12 on the pain scale of 1 – 10, which no positioning or over the counter pain medication can touch had me rolling on the floor and telling the kids to call Dad to come home from work now.
Yes, that was just the beginning of my kidney stone experience. In trying to explain the pain to my husband on the phone, he said I sounded so short of breath that he thought I was having a heart attack and called EMS. When they arrived, the pain had subsided and I was left to diagnose myself with a kidney stone, with which the paramedics agreed. But since the pain was completely gone, did I really need to go to the hospital and in an ambulance no less? On their recommendation, the answer was yes.
In the ER, the IV was started and a CAT scan done to confirm our suspicions. Having no history of kidney stones, I was surprised at this painful attack that came on with no warning at all.
The ER doctor came in to see us and said in a thick accent, “Well, you were right. In 5 – 7 days you will have a special delivery!” he laughed.
I glanced at my husband who had turned white and later told me he thought for a second, “you mean she’s having a baby?!” (which at 53 surely would have been some sort of miracle). My first thought was “5 – 7 days of this pain? Are you kidding me?” How will I survive?
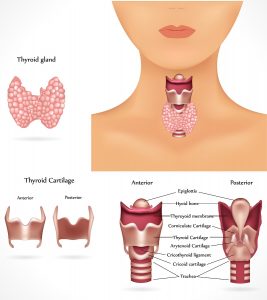
Another painful bout came as I lay on the gurney, and four strong IV medications didn’t completely take away the pain. We were told the pain comes from the spasms of the ureter as the stone blocks the flow of urine and irritates the inflamed tissues. Who could imagine that a 2 mm stone the size of a grain of sand could cause so much discomfort? The word intractable pain had new meaning for me now and I wished I had been more sympathetic to people and patients with kidney stones.
They sent us home with a urine strainer and prescriptions for Flomax and a combination of anti-inflammatories and pain medications. Another attack in the car and all I could do was writhe in pain and pray for relief. My husband kept repeating, “I hope I never get one of those”. It is the type of pain that one would do almost anything to stop but that nothing relieves short of passing the stone.
As I took my pain pills, strained my urine, and drank copious amounts of water to help the delivery along, I had time to reflect on the age old debate of kidney stone pain being akin to labor and childbirth. Having some experience in the childbirth area, I still found no way to compare the two in terms of what hurts more, but here were my reflections:
Labor pains were more predictable and increased with intensity as you moved towards the goal of delivery. Kidney stone pain, on the other hand, was unpredictable and had the most intense pain with every bout.
Doctors can predict when the baby will be delivered by closeness of contractions, and examining cervical dilation and effacement. Kidney stone delivery is much less predictable.
If your baby is too big to be delivered vaginally or there are complications, a C-section can be performed. And if your kidney stone is too big to pass, you may have laser treatment to break up the stones or major surgery to retrieve them. Both can mean painful recoveries.
There are medications they can give you for labor and delivery. You can even get an epidural, which I never had, but am told they can make the experience much less painful. But the kidney stone pain didn’t seem to be completely obliterated by anything short of passing it.
In comparing types of pain, I guess I can see where men would say they come close to labor pain with a kidney stone, but 10 hours of back labor was equally as bad, and having your OB doctor turn your baby internally prior to a natural birth still rates as the #1 pain I have ever had (but at least it was over quickly).
And last, but most significantly, with labor and childbirth you expect and usually earn a wonderful, lasting, happy surprise at the end of the process, where you hold your newborn in your arms and experience the glory of motherhood, quickly forgetting the pain that was endured to have your bundle of joy. Whereas, at the end of your kidney stone passing, you collect a little grain of something that goes into a plastic container for the urologist to later analyze and you can’t believe how much that little devil hurt to get out. You may experience relief and joy at the passing, but there are lifestyle modifications to make to try to avoid it ever happening again, and still without the assurance that it can be prevented, so unlike the conception process. Who, having had one kidney stone, would ever make plans to have another?
Fortunately, my stone did not take 7 days to pass and was gleefully collected in a matter of hours.
So, my answer to the question of which is more painful, a kidney stone or labor and delivery, is a simple one: they cannot be compared. It’s like apples and oranges. Different types of pain, but both extremely intense, though the kidney stone is much more unpleasant because the outcome is not a lasting joy for the rest of your life. Since every person experiences pain differently, no one could really answer this question anyway because pain is a subjective experience.
For me, given the choice between labor and a kidney stone, I pick labor. Childbirth is definitely more fun and with rewards that last a lifetime.